Lung allocation based on the Composite Allocation Score (CAS): Questions and answers for patients and caregivers
This page was printed on:
Welcome to our question-and-answer page for the new lung allocation policy that took effect March 2023. This policy uses an approach known as continuous distribution. Continuous distribution is predicted to improve the organ matching process by considering all factors about each transplant candidate in a single score.
Below are answers to the most common questions from people seeking a transplant for themselves or a loved one. If you have a more general interest in transplantation, we hope you find it helpful as well.
The team at your transplant hospital will always be your first and most complete source of information regarding your current medical condition and treatment options.
If you have other questions or comments, contact the Organ Procurement and Transplantation Network (OPTN) Patient Services line at (888) 894-6361 or submit them here.
Every lung transplant candidate receives an individualized lung Composite Allocation Score (CAS). This score determines priority for receiving a lung transplant when donor lung(s) become available. The lung CAS is individual for each patient and each organ offer. The lung CAS point values represent each of the factors used to match organ offers with transplant candidates. The people who have the highest number of points for that organ offer will have the highest priority.
How is the lung CAS calculated?
The lung CAS uses objective medical information about your needs and medical condition. It also uses objective medical facts about the potential organ donors that may be a match for you. The score weighs the different factors used to make the match. This means each factor will get a certain number of potential points, which are then added together to make up a maximum score of 100 points. Some factors are more important in matching and will be worth more points within the overall score, while others get fewer points. Medical experts have carefully determined the weight for each factor based on input from the donation and transplant community as well as detailed statistical information. Patients and the general public also provided input on the factors that they think are most important in determining how to place donor lung(s).
The lung CAS uses a framework called continuous distribution. Some of the goals of this framework are to:
- Prioritize sickest candidates first to reduce waitlist deaths
- Improve long term survival after transplant
- Increase transplant opportunities for patients who are medically harder to match
- Increase transplant opportunities for candidates with distinct characteristics like candidates under the age of 18 or prior living donors
- Promote the efficient management of organ placement
Lung CAS animated explainer video
Learn how the lung Composite Allocation Score (CAS) is calculated and used in lung allocation in this brief animated video.
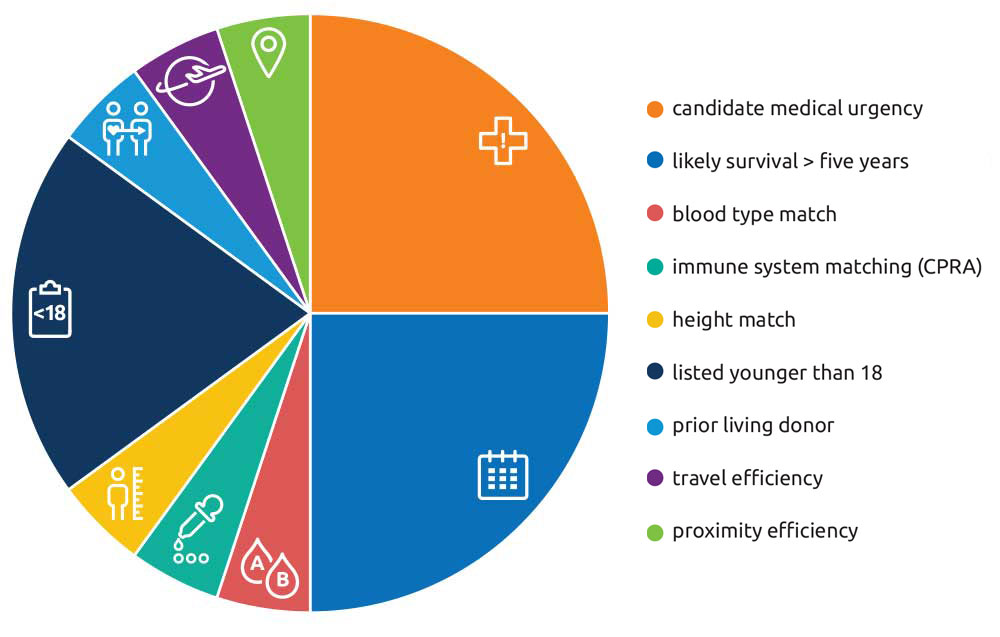
Half of the lung CAS (up to 50 points) comes from medical urgency and likelihood of survival at least five years if transplanted:
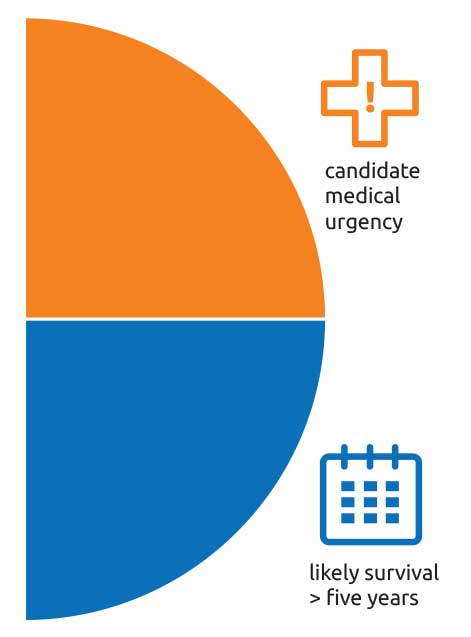
- Up to 25 points are based on each candidate’s medical urgency – how quickly you may need a transplant.
- In addition, up to 25 points are based on the candidate’s likelihood of surviving at least five years if transplanted.
Next, as many as 15 points are reserved for candidates who are hard to match for some or most organ offers. This extra priority is meant to give more opportunities for lung offers that could be a match.
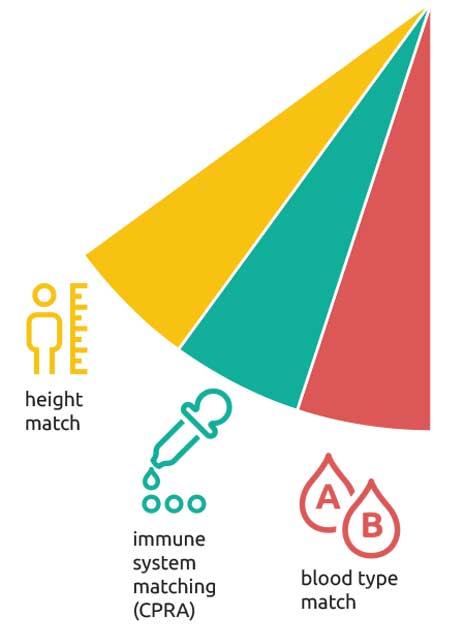
There are three categories, each of which make up as many as 5 points toward the overall lung CAS:
- Up to 5 points are based on each candidate’s blood type.
- Candidates who have harder-to-match blood types with potential donors receive more points than those with more common blood types.
- Up to 5 points are based on the candidate’s calculated panel reactive antibody (CPRA) score
- CPRA is a medical test that measures immune system antibodies a candidate has that prevents them from accepting certain donor lung(s).
- For example, a person with a CPRA score of 80 could not be a match with organs from 80 percent of donors. Patients with a high CPRA score (harder to match) get more points to qualify for offers that may match them. People with a low CPRA score (easier to match with most donors) receive fewer points, or none at all, in this category.
- CPRA is a medical test that measures immune system antibodies a candidate has that prevents them from accepting certain donor lung(s).
- Lastly, in this category, up to 5 points are based on the candidate’s height.
- Donor lung(s) must be a reasonable size match within the patient’s chest. Patients who are much shorter or taller than average tend to get fewer matching lung offers than those who are of more common height. For this reason, candidates who are either very short or very tall receive more points in order to have better access to donors that could be a match.
Next, up to 25 points are reserved for candidates who have special needs for access to a transplant:
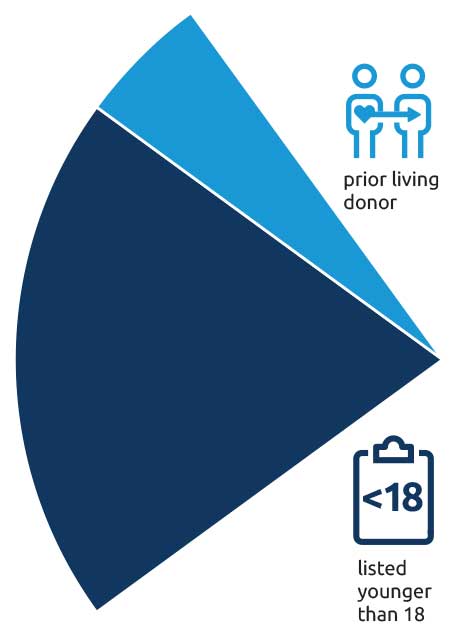
- Candidates younger than 18 years old at the time of transplant listing will receive 20 points.
- Candidates who were living organ donors will receive 5 points.
The final portion of the CAS, worth as many as 10 points, reflects the effort needed to preserve and transport the lung(s) from the donor to the recipient hospital. Lungs are only viable for a few hours between donor and recipient. The shortest possible travel time and distance often boosts the chance of a successful transplant.
There are two parts to assigning points for the transportation of donor organs, each of which can be as much as 5 points:
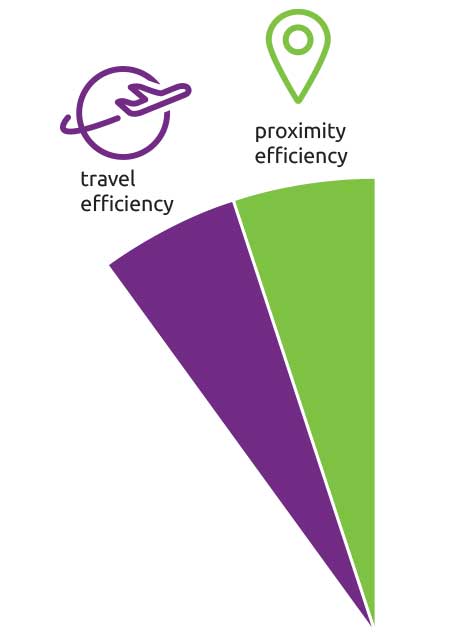
- Up to 5 points are based on travel efficiency.
- This estimates the type of transportation and expense needed to transport donor lung(s) from the donor hospital to the transplant hospital. Donor/candidate matches with the greatest travel efficiency are assigned the highest number of points.
- For example, if the donor and candidate are within the same hospital or at very nearby hospitals, or if the lung(s) can be transported by road instead of flight.
- This estimates the type of transportation and expense needed to transport donor lung(s) from the donor hospital to the transplant hospital. Donor/candidate matches with the greatest travel efficiency are assigned the highest number of points.
- In addition, up to 5 points are based on proximity efficiency.
- This estimates factors other than travel in transporting donor lung(s). Organ offers with the least complicated arrangements receive the highest number of points.
- For example, matches that result in the shortest possible travel time between donor and transplant hospital.
- This estimates factors other than travel in transporting donor lung(s). Organ offers with the least complicated arrangements receive the highest number of points.
Could any person have a CAS of 100?
No, transplant candidates could never get the total maximum score for each factor. For example, no one person would be under age 18, be a prior living donor, and also have the maximum disadvantage in terms of height, blood type and CPRA level.
For some attributes, if you do not qualify, you will not get any points for that item within the total score. For example, if you are not a prior living donor, you would not get any of the points reserved for living donors. Similarly, any transplant candidate listed after age 18 will not get any points reserved for pediatric status.
For other factors, you might receive some number of points, but not always the maximum amount. For example, a person might get one point based on height disadvantage, 5 points based on blood type and one point based on CPRA score, totaling 7 out of a possible 15 points.
For the parts of the lung CAS that do not depend on the specific organ offer, many candidates will have scores around 20 to 25. In rare cases, candidates may have a lung CAS as high as 40 to 45 before points are added for the logistics of the match with the donor.
Because the distance from donor to transplant hospital accounts for as much as 10 points within the total lung CAS, you will not have the same score across all organ offers. Your score could be lower on one match run for a donor at a hospital 500 miles from your transplant program, then very high on a match for the next donor at a hospital 50 miles away.
How is the lung CAS used in organ offers? What if I have the same score as someone else?
The OPTN’s computerized matching system gives the highest priority to the candidates with the highest total CAS for each lung offer. If the offer is not accepted for the person with the highest CAS, it will then go to the candidate with the next-highest score. The offers will be made in that order until a transplant program accepts the offer, or until, for whatever reason, the lung(s) cannot be transplanted. Remember that part of your lung CAS will be how far your transplant hospital is from the donor hospital, so it will not be the same for every available organ.
Under extremely rare circumstances, it is possible that two or more candidates will have the same exact lung CAS. If there is a tie among candidates, waiting time for transplant is used as a tiebreaker. The person who has been listed longest for a transplant would receive an organ offer before others with the same lung CAS but who have been listed a shorter time.
These two factors make up half (a maximum of 50 points) of the total lung CAS. They are split evenly into medical urgency (up to 25 points) and expected post -transplant survival (up to another 25 points). Keep in mind that most candidates do not receive the maximum score totals available for either component.
A set of medical tests or observations are put into a formula (see list on the following page). These are proven statistically to affect how soon people need a transplant and how likely they would be to survive at least five years after a transplant.
In addition, each candidate age 12 or older is included in a diagnosis group that represents their need for a transplant. There are four diagnosis groups. Each of those groups has been shown statistically to have similar patterns of medical urgency and post-transplant survival. As a result, each group gets a different amount of weighting in the lung CAS formula to represent how that group of diseases affects overall medical urgency and survival rates.
What do I do if my child has an adolescent exception?
The lung CAS applies to all transplant candidates, regardless of their age. Therefore, there is no need for an adolescent exception in order to ensure access to specific types of donors. Additionally, all candidates added to the list before they reach 18 years of age will receive 20 points based on their pediatric status.
What tests/observations are used to determine urgency and expected survival?
- Oxygen at rest: The amount of oxygen needed at rest to maintain enough oxygen in the blood. People with severe lung disease may need additional oxygen.
- Age: Age at the time lung(s) are offered.
- Body mass index (BMI): A measure of body fat based on height and weight. When combined with other medical test results, BMI assess health status.
- Functional status: A way to measure the effects that lung disease has on performing routine daily tasks.
- 6-minute walk distance: How far you can walk in 6 minutes is a measure of functional status.
- Assisted ventilation: An external device connected directly to the patient to help move air into and out of the lungs. The use of a ventilator to aid breathing is a measure of how sick the patient is.
- Serum creatinine: A measure of kidney function. High creatinine levels mean a patient’s kidneys are not working well, which sometimes happens along with severe lung disease.
- Diagnosis: Different kinds of lung diseases vary in how effective a lung transplant is in treating them. Therefore, diagnosis is part of the composite allocation score.
- PCO2 and change in PCO2: The amount of carbon dioxide in the blood. When the lung isn’t able to exchange oxygen and carbon dioxide as it should, the PCO2 level may increase.
- Bilirubin: A substance made by the liver when it breaks down old red blood cells. High bilirubin is a marker for right heart failure that can occur with lung disease.
- Cardiac index:A measure of how well the heart is pumping blood. A low cardiac index means the heart is not keeping up enough blood circulation. Note: This is used in calculating the post-transplant portion of the score, but not for waitlist urgency.
Children younger than age 12, are listed either as Priority 1 or Priority 2 based on measures of their current level of illness. The criteria for each of these statuses will not change from the current policy.
The factors used to calculate medical urgency and transplant outcome for candidates age 12 and older do not apply to patients younger than 12. For this reason, their scores will be different and will be a fixed value based on their priority status.
Priority 1 candidates have a higher level of medical urgency than those who are Priority 2. Thus, Priority 1 will have a higher fixed score for medical urgency (1.9073 points) than Priority 2 (.4406 points).
The part of the score addressing post-transplant outcome will be the same for all candidates younger than age 12, regardless of priority. It will be a fixed amount of 18.6336 points.
Not always. The OPTN matching system sets the order of candidates to get lung offers. However, the offer may not be accepted for the top-ranked person or even for a number of others. Reasons for deferring an organ transplant vary, but they can include:
- The patient’s inability to be transplanted at the time of the offer
- Medical facts about the donor (such as age, size or quality of the lung(s) likely organ transport time, transmissible disease risk, etc.) that may affect the success of transplanting the particular patient getting the offer
The medical staff at your transplant program reviews detailed medical information about the donor for all lung offers identified for you. The transplant team makes the final decision to accept or turn down any offer. If the organ is not accepted for the first patient on the match, it is then offered to the next candidate. This continues until a match is found, or until the lung(s) can no longer be placed.
The reasons can vary for lungs that can no longer be transplanted. They include, but are not limited to:
- A medical complication(s)
- A downward trend in organ function
If your transplant team believes that your lung CAS does not truly reflect your clinical situation, they may ask a group of expert reviewers, known as the Lung Review Board, to review your situation.
The Lung Review Board considers the information provided and assess how your condition compares to other candidates who have the score your team is requesting. The board then decides whether to approve or deny the request. Keep in mind that since the lung CAS combines a number of factors, the board may approve an adjustment in one or more parts of the score (for example, an increase in medical urgency priority) while other parts remain the same.
What is the Lung Review Board?
The Lung Review Board is a national group of transplant physicians and surgeons, established by the OPTN. The board, which consists entirely of volunteer subject matter experts, reviews requests from transplant hospitals to grant priority in exceptional cases. These requests are created when the transplant team believes that the assigned score does not represent the severity of the case. The Lung Review Board looks at the medical facts of each case and decides whether to approve or deny the request. Members of the board do not see names or details that identify the patient or hospital.
In general, your transplant team will update your medical information at least every six months. Your transplant program already collects most of the needed information on a regular basis.
If you are receiving some form of highly advanced treatment that usually requires you to be in the hospital, your program must update those lab values at least once every 28 days. This will ensure your score reflects the most updated information about your condition.
Your hospital may also update your information in the system any time your transplant team thinks it is necessary to reflect a change in your condition.
This system has been improved over time, and it will continue to be studied for further improvement. In organ transplantation, as in all scientific fields, new studies are taking place all the time to learn how to save more lives.
In fact, this policy was designed to allow faster and simpler improvements, such as changing the weight of one or more factors in the lung CAS. Your transplant team will keep you informed of changes to the system and what you may need to do.



