Living donation
This page was printed on:
Welcome to our question and answer page on living donation.
Below is commonly requested information regarding living organ donation. We hope you find it helpful.
If you have other questions or comments, contact the Organ Procurement and Transplantation Network (OPTN) Patient Services line at (888) 894-6361 or submit them online here.
What is living organ donation?
Living organ donation is when a living person donates their organ or a part of their organ to transplant into another person.
Most living donors donate one of their kidneys or a part of their liver. Other organs can be donated by living donors, but are much rarer.
Living organ donors make thousands of transplants possible every year. There is a lot to learn before you decide whether donating an organ is right for you. This brochure contains information about living kidney and liver donation. Talk to staff at a transplant hospital if you would like to learn more about other types of organ donation.
As a living donor, you can shorten the wait for a transplant patient
In the United States, the demand for organs exceeds the supply of donated organs. Many people wait years for an organ from a deceased donor.
Only about half of the people in the United States sign up to donate their organs when they die. This number is different in every state and region, so the wait can be longer depending on where someone lives.
Every year, thousands of people get removed from the waitlist because they have become too sick to have a successful transplant.
To shorten the wait, family, friends, co-workers, and even strangers can offer to be living organ donors.
Living donor transplants can help shorten or eliminate the wait for an organ by:
- Giving transplant candidates more options to plan.
- Helping kidney transplant candidates get an organ transplant before they need to begin dialysis.
Living organ donors make thousands of additional transplants possible each year.
Living organ donors can improve the chances of transplant success
Kidneys from living donors generally have high success rates:
- More than 98% of transplanted kidneys from living donors are still working one year after transplant.
- On average, living donor kidney transplants work longer than kidney transplants from deceased donors.
Living donor liver transplants also have as good or better outcomes compared to liver transplants from deceased donors.
Only you can decide whether living donation is right for you
No one can make the decision to donate for you, and no one should pressure you.
Before you decide, learn as much as possible about living donation so you know the risks and benefits. This brochure gives basic information about living donation. The best place to learn is at a transplant hospital. Talk to transplant hospital staff to learn more.
When you learn about living organ donation at a transplant hospital, bring family or friends with you.
Including your family or friends will:
- Help you remember what the transplant hospital staff teaches you.
- Help you think of questions to ask.
- Let your family and friends know the best way to help you.
Can I be a living donor?
To be a living donor, you must:
- Be an adult (over age 18) able to make an informed decision
- Be in good physical and mental health
- Understand the risks and benefits of living donation
- Decide for yourself whether living donation is right for you
Both you and the transplant hospital staff have to decide whether living donation is right for you. The transplant hospital staff will need a lot of information about you to make sure you are healthy enough to donate.
To help decide whether donation is right for you, transplant hospital staff will:
- Give you a full physical examination and medical tests
- Ask about your medical history
- Ask about your social support
- Assess your mental health
- Ask about your finances and whether you can take time off from your commitments
- Inform you about the risks and benefits of living donation
- Make sure that your decision to donate is yours alone
Certain health issues may cause the transplant hospital staff to decide you should not donate an organ. This is for your health and safety. Here are some examples of such health issues:
- Uncontrolled high blood pressure
- Untreated psychiatric condition
- Cancer
- Diabetes
- Certain infections
Do I have to know the person to whom I donate an organ?
Giving an organ to a specific person is called directed donation
In directed donation, a donor who is medically compatible may be:
- A blood relative of the transplant recipient, such as a parent, brother, sister, or adult child
- Someone close to the transplant recipient, such as a spouse, a friend, or a co-worker
- Someone who the donor has heard about but does not know personally
Non-directed donation is when you want to donate but do not know - and may never know - the person to whom you will donate
In non-directed donation, the donor may be:
- Someone wishing to donate to a stranger on the transplant waitlist
- Someone who begins the process to donate to a friend or family member but later decides to donate to a stranger after the friend or family member gets an organ from someone else
A transplant hospital can match a non-directed donor to a transplant candidate who is a match. Sometimes, a match happens through a paired kidney exchange. Kidney paired donation helps more transplants happen. That process will be explained later.
Some non-directed donors wish to meet their transplant recipient. Sometimes that happens and sometimes it does not. It is a personal choice. The transplant hospital will help make a meeting happen only if the living organ donor and the recipient both wish to meet.
What if I want to donate my kidney to a specific person but we do not match?
Sometimes, someone wants to donate a kidney to a specific person but tests show the two people are medically incompatible. That can happen because of different blood types or other test results that show the kidney has a high risk of rejection. There are still ways you can donate, including:
Kidney paired donation (KPD) is when a computer matches donors and recipients to create compatible pairs. Think about it as a swap or an exchange. Here’s how it works:
- You want to donate a kidney to someone, but you are not medically compatible.
- Another person wants to donate a kidney to someone, but they also do not match.
- A computer matches you with a compatible recipient, and their donor matches with the person you want to help.
- Swapping donors allows both transplants to happen.
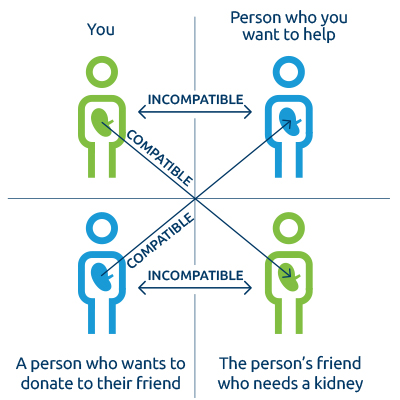
KPD allows hundreds of people to get a transplant each year. The person you want to help may get a transplant more quickly in an exchange.
How do I start the process to become a living donor?
The process starts at a transplant hospital.
- If you want to donate to someone you know, such as a family member, friend, or co-worker, ask that person to put you in touch with their transplant hospital.
- If you want to donate to someone you know but want to get tested before telling the transplant candidate, talk to their transplant hospital. Many transplant hospitals will test you without telling the transplant candidate.
- If you want to donate an organ to someone you do not know, call a transplant hospital near you to talk about it.
Find a list of transplant hospitals.
Will someone at the transplant hospital help me with the process?
If you and the transplant hospital staff agree that it makes sense for you to be evaluated, the transplant hospital staff will put you in touch with an independent living donor advocate.
An independent living donor advocate’s job is to protect you. Their job is not to think about what the transplant candidate needs or make transplants happen. The independent living donor advocate will:
- Protect you and your best interests
- Support your rights, such as making sure you have the time and information you need to decide whether donating is right for you
- Make sure you know the risks and benefits of living donation
- Help you walk away if you decide living donation is not right for you
The independent living donor advocate will make sure you have information about:
- Consent: When you agree to give medical information and undergo testing
- Evaluation: What tests you need to take and why
- Medical and psychosocial risks: Possible problems you may have during or any time after donating, including coverage for childcare or eldercare
- Financial risks: Issues with expenses, work, or insurance
- The surgery: What to expect the day of the operation and the risks
- Recovery: What to expect after surgery and getting back to normal activities
- Medical follow-up: Tests you are required to have after you donate
Independent living donor advocates want you to share anything that is on your mind. If you have fears, concerns, or second thoughts, your living donor advocate wants to know. Sharing your thoughts is the best way to help your living donor advocate support you and help you decide what is right for you.
The advocate will not share your medical or other information with the transplant candidate.
Step 1: Consent to be tested and provide health information
When you call a transplant hospital, a living donor staff member will briefly explain the donation process and ask if you agree to give some information about your health. Your consent begins the evaluation process.
Different transplant hospitals might ask you about your health in different ways:
- Online
- Over the phone
- In person
Your answers help the transplant hospital team decide whether to continue to the next step. Some health issues are minor and donation may still be possible.
Transplant hospitals may have different opinions about certain health issues and their risks. Transplant hospital staff will explain their opinions to you.
Step 2: You and the transplant hospital start a careful evaluation process
If you and the living donor team both decide to continue, you’ll start a wide-ranging evaluation process. The purpose is to protect you and the potential transplant recipient. It also helps to make sure a transplant is likely to have a good outcome.
The transplant staff members ask questions about all areas of your life, such as:
- Why do you want to donate?
- How do you think donating will affect your life? Your family?
- Can you afford the non-medical expenses, like travel?
- Who will help you afterwards?
- Can you afford time away from commitments?
- Do you have any risky habits or behaviors?
Some of the questions are really personal. The purpose is to make sure donation is safe and right for you.
Be sure to ask any questions you have. There is no such thing as a bad question or too many questions. Answering all of your questions is one of the most important jobs of the living donor team. Bring a family member or friend with you to help you remember everything you need to know.
What tests will I have during my evaluation?
To make sure you are healthy enough to donate, you will take a lot of tests. The purpose of testing is to protect you.
Some of the tests also give information about the likelihood of a good transplant outcome if you become a living donor. Your medical information and test results are confidential. By law, transplant hospitals cannot share your medical information with the transplant candidate without your permission.
Here is a list of the kinds of tests living donors have to take. Each test will be described below.
- Psychosocial evaluation
- Blood tests
- Heart and lung tests
- Tests of the organ to be donated
- Routine health tests
Psychosocial evaluation
Living donor team members will ask you questions about your life. This helps you and the transplant hospital staff decide whether living donation is right for you. Here are some examples of the questions:
- Why do you want to donate?
- Do you feel pressure from anyone to donate?
- How well do you understand the process, risks, and benefits so that you can make an informed choice?
- Will donating affect your job? Your finances?
- How might donating affect other parts of your life, such as caring for a child or a parent?
- Who will help you during recovery?
- What are your family’s views about your donation?
- Do you have any mental health issues that could be made worse by donating?
- How do you think you will feel after donating?
- How do think you will feel if things do not go as you hope they will?
Blood tests
Some blood tests give the transplant hospital staff information about your health. Other blood tests show the staff whether you are a match with a transplant recipient.
- Blood type compatibility: Blood tests let the transplant hospital know whether you and a transplant recipient have compatible blood types.
| Donor blood type | Recipient blood type |
|---|---|
| O compatible with: | O, A, B, and AB |
| A compatible with: | A and AB |
| B compatible with: | B and AB |
| AB compatible with: | AB |
- Tissue typing: This blood test checks the tissue match between you and a transplant candidate. Transplant hospital staff use this information in caring for the transplant recipient. Even if you and the recipient are not tissue matched, the recipient can still have a successful transplant because of medications to combat organ rejection.
- Cross-matching: This blood test checks for factors associated with increased risk of organ rejection by the transplant recipient.
- Transmissible diseases: These blood tests look for infections or conditions that a living donor could spread to the transplant recipient. The law requires medical staff to report certain infections confidentially to public health officials.
Heart and lung tests
- A chest x-ray, an electrocardiogram, and other tests will be conducted to make sure your heart and lungs are healthy enough for you to be a donor.
Tests of the organ you wish to donate
- CT or MRI scan to let the transplant hospital staff look at the organ you wish to donate.
- Kidney donors have blood and urine tests that give information about their kidney health.
- For liver donors, some transplant hospitals use a small needle to take a tiny piece of the liver to make sure it is healthy enough to donate.
Routine tests depending on your age and the tests you have had in the past
- A colonoscopy
- Skin cancer screening
- Gender-specific exams
Not all transplant hospitals require the same tests. Your transplant hospital staff will explain what tests you need. They also will explain why the tests are important.
Getting through all the tests takes time. If you are donating to someone whose hospital is far away, you may be able to do some of the medical tests closer to your home. Talk with the transplant hospital staff about options.
Who decides if I may donate?
If you pass the evaluation process, the final decision about whether you will donate is yours.
Your decision must be informed and voluntary.
An informed decision means you understand:
- The donation process
- The risks and benefits of donation
- The other options a transplant candidate might have, such as dialysis or transplant from someone else, living or deceased
A voluntary decision means you:
- Feel no pressure from anyone to donate
- Know you may decide not to donate at any time
- Are not expecting a promise of money or anything of value
When you think about whether to donate, it is helpful to talk with people
The decision to donate is not easy. There is a lot to think about. Donation could impact your health, your family, and your work. Sometimes people offer to donate an organ before they learn about the risks and benefits. After learning more, some people decide that donating is not right for them. They may worry about letting someone down.
Talking through your thoughts can help. Talk with family members, close friends, or anyone you know who is a good listener. You may also want to talk with living donors. Transplant hospital staff can help find living donors who would be happy to share their experience with you.
Other organizations, like the National Kidney Foundation, can put you in touch with a donor. Call the National Kidney Foundation’s PEERS Program at (855) 653-7337 (855-NKF-PEER) or email nkfpeers@kidney.org.
The most important thing is that you do what you feel is right for you.
People may decide not to donate for many reasons. Your decision to donate or not, and the reasons for your decision, are yours to make.
If you decide not to donate at any point, for any reason, talk with your transplant hospital social worker, donor coordinator, or your independent living donor advocate. These staff members are there to help you. They want to hear your thoughts, concerns, and feelings. The transplant hospital staff will keep your reasons for deciding not to donate private. They can help you think about what to say if people ask questions about why you are not able to donate.
What are some of the risks if I donate?
When someone donates any organ, there are different kinds of medical risks.
- Immediate risks: During or right after surgery
- Short-term risks: In the year or so after surgery
- Lifetime risks: Anytime during your life
The transplant hospital staff will explain all the different risks of living donation.
Your transplant hospital staff will talk with you about:
- How likely the risks are to happen
- Whether the risks are serious
- Whether the risks are in the short-term or could happen at any time
- Whether and how the problem would be treated
Risks differ from person to person.
Every surgery has risks. Here are some examples of the problems that are possible during or right after kidney or liver donation surgery:
- Pain
- Infection
- Bleeding
- Blood clots
- Injury to tissue or other organs
- Pneumonia
- Allergic reaction to anesthesia
- Death
When someone donates a kidney, they live with one kidney for the rest of their life. With one kidney instead of two, living kidney donors have reduced kidney function. Here are some of the possible risks of kidney donation:
- Hernia
- Organ failure (needing treatment or possibly transplant)
- New or ongoing high blood pressure
- High blood pressure after pregnancy
When someone donates a part of their liver, the part they keep and the part they give to a transplant recipient both grow to almost full size. Here are some of the risks of liver donation:
- Wound infections or hernia
- Bile leakage
- Intestinal problems (blockage)
- Organ failure (needing treatment or possibly transplant)
Remember, the best place to learn about risks is from your transplant hospital staff. If you hear about other possible risks, always go back and talk to your transplant hospital staff. When you make your decision, you need facts. Your transplant hospital is the best place to get them.
Not every possible lifetime risk is known
Your transplant hospital staff will give you some information about the lifetime risks of living organ donation. However, transplant hospital staff cannot tell you every possible long-term risk. Based on the best information known so far, overall risks to health are considered to be low for those determined to be healthy enough to donate.
Donating is a lifetime decision. All living donors should commit to a lifetime of healthy habits and healthcare. Living donors need to have medical follow-up care after donating. Living donors also should go to their local doctor for a health check-up every year. You can manage health risks by taking good care of yourself and controlling things like your blood pressure and weight. Your doctor can help you.
How might I feel after living organ donation?
About 90 to 95 out of every 100 donors say they would not change anything about their decision to donate.
They would make the same decision to help someone. They would go through all the screenings, tests, and surgery. They would take time away from their lives, jobs, and other commitments to recover. They would do all of that to help someone.
They feel good about extending the transplant recipient’s life. They feel satisfied about improving the transplant recipient’s quality of life.
Sometimes, living donors feel regret or resentment. Some say they feel depressed. This can happen even years after donating. Some examples are when:
- A donated organ does not work well in the recipient after transplant surgery
- The donor or the transplant recipient has medical problems after surgery
- The donor’s scars do not fade as much as the donor expected
If this happens to you, you may need support from a professional to work through these feelings. Be sure to talk with the transplant hospital staff in advance about these and other risks. If you donate and have concerns afterward, ask your transplant hospital or independent living donor advocate to help you find support.
How long does it take to get back to normal life after donating?
After surgery, living donors need time and help from family and friends before getting back to routine activities. Here are some tasks and the average time living donors take to return to each.
| Kidney donors | Liver donors | |
|---|---|---|
| Stay in the hospital | about 2-3 days | about 5 days |
| Drive a car | about 2 weeks | about 2-4 weeks |
| Get back to pre-donation activities | about 4-5 weeks | about 8 weeks |
| Lift heavy items | about 6-12 weeks | about 8-12 weeks |
Every donor is different. Some donors get back to their lives quickly. Others say they feel tired for quite a while after donation. Since you do not know how you will feel, it is important to have family and friends ready to help you for as long as you need. If you take more time than other donors, let your transplant hospital staff know.
Will I need follow-up medical care after I donate?
After you donate an organ, you need to take good care of yourself and have yearly medical check-ups with your doctor.
“Everyone says I gave the gift of life when I donated. Doing my follow-up and seeing my doctor every year to make sure I’m ok is also a gift. It’s a gift I give to myself and my family.” – Ron
All living donors need certain tests six months, 12 months, and 24 months after surgery, but these may vary according to the transplant hospital. Ask the transplant hospital staff:
- What tests will be done
- Where the tests will happen – at the transplant hospital, a local lab, or at your own doctor’s office
- Who will pay for follow-up
Sometimes, even if you feel well, tests may show you need treatment. Follow-up is very important. Transplant hospitals must track and report to the OPTN whether you get the tests you need after you donate.
Check-ups help the transplant hospital staff make sure you are healthy. They give you a chance to talk about how you feel and what you might do to be as healthy as you can be. Your follow-up also gives transplant hospitals information that can help future donors.
Commit to your required follow-ups after donation and see your family doctor every year.
Who pays the costs if I decide to donate?
Before you decide whether to donate, learn about all the possible costs and which, if any, you may have to pay. Transplant hospital staff will talk with you about living donation expenses and how they are usually paid.
A transplant candidate’s insurance generally covers a living organ donor’s medical expenses.
These expenses include a donor’s evaluation, tests, and surgery. Talk to your transplant hospital staff if you need help paying for other tests you may need to have done (colonoscopy, or a mammogram for women, or a prostate exam for men).
The transplant candidate’s insurance is not likely to cover other costs, such as:
- Medical care if your evaluation shows that you have a disease that needs to be treated
- Long-term medical care if the donation causes you problems
- Follow-up care for the rest of your life
Every insurance policy is different. Be sure to ask questions about what medical costs may not be covered by insurance.
Some transplant patients have Medicare. Sometimes Medicare may help living donors who have donation-related complications. For more information, contact Medicare at 1-800-MEDICARE or at medicare.gov.
Think about your health insurance situation
Some transplant hospitals require living donors to have health insurance.
Most living donors do not have problems with insurance because of donating. After you donate, an insurance company may consider you to have a pre-existing condition. If that happens, it is possible that:
- It could be harder to get new health, disability, life, or long-term care insurance.
- It could be harder to increase your life insurance coverage.
- Your premiums might be higher than they would be without a pre-existing condition.
Federal law may protect living donors from problems with health insurance. Talk with a social worker at the transplant hospital about risks and ways to protect yourself.
Check with your employer about other benefits that may help you
If you are employed, talk with your employer about other benefits that could be helpful. These include:
- Vacation time
- Disability pay
- Sick time
- Leave of absence
Talk with your transplant hospital staff if you need help with non-medical costs, such as travel and lodging.
You may be able to get help with costs for travel expenses, lost wages, and dependent care during testing or surgery. The National Living Donor Assistance Center (NLDAC) helps some donors with these kinds of expenses based on eligibility. Contact the NLDAC toll-free at 1-888-870-5002 or go to livingdonorassistance.org for more information.
A transplant recipient, family members, a transplant hospital, or charities also may be able to help you with certain non-medical expenses.
Ask your transplant hospital social worker to explain what kind of help you can accept. It is illegal to give or take money or anything else of value, such as a gift or a vacation, in exchange for donating an organ.
Can I get information about living donors?
The OPTN collects data about living donors from transplant hospitals across the country. Looking at data may help as you think about whether or not to donate.
Talk with your transplant hospital staff about the data to find out what it really means for you.
Transplant hospitals give the OPTN information about medical problems living organ donors have in the two years after surgery. Serious problems are rare.
Here are a few examples of living organ donor data:
To find data about living donation at your transplant hospital or elsewhere, visit the OPTN’s Data Reports page. You can also find more information at the Scientific Registry of Transplant Recipients website.
Understanding data is not always easy.
Talk with your transplant hospital about the following living organ donor data:
- Number of living organ donor surgeries
- Percent of living donors who had medical problems
- Percent of living donors who participated in follow-up
- Living organ donor transplant recipient outcomes
Where can I get more information?
You can learn more by contacting the OPTN Patient Services line at (888) 894-6361 or emailing Patient.Services@unos.org.
The Department of Health and Human Services required the OPTN to develop living donor guidelines and policies in 2006. Find policies that impact living donors on OPTN’s Policies page. You also can submit your feedback on current policy proposals on the Public Comment page.
Useful websites
- U.S. Department of Health and Human Services
- List of U.S. transplant hospitals
- National Kidney Foundation
- American Liver Foundation
- National Institutes of Health
- National Living Donor Assistance Center
- United Network for Organ Sharing (UNOS)
Acronyms and terms
Colonoscopy - An examination of the colon using a flexible fiber-optic device inserted through the rectum.
CT scan - A procedure using a computer linked to an X-ray machine to make a series of 3-D images of areas inside the body.
Electrocardiogram - A test that measures the electrical activity of the heartbeat.
Immunosuppression medications - A class of drugs that reduce the strength of the body’s immune system, making it less likely to reject a transplanted organ.
Mammogram - An X-ray picture of the breast.
MRI scan - Uses a large magnet, radio waves, and a computer to create detailed images of internal organs and structures.
Prostate - A gland in men that surrounds the urethra, the tube through which urine passes out of the body.
Types of living organ donors
Compatible donor - A person whose blood and tissue type and other medical factors match with the recipient.
Deceased donor - A person who has been declared dead by brain death or cardiac death and whose organs are healthy enough to be used for organ transplant.
Incompatible donor - A person whose blood type or other medical factors do not match with the recipient. An incompatible donor may still be able to donate through exchange programs (kidney paired donation) or incompatible transplantation programs.
Living donor - A person who is alive when they donate an organ, usually a kidney or a part of their liver. Living donors are healthy and undergo many medical tests before they are allowed to donate an organ.
Non-directed donor - A person who wants to donate an organ but does not have a specific recipient in mind. A non-directed donor expresses interest in donating to a transplant hospital. Non-directed donors are sometimes called anonymous donors or altruistic donors.
Paired donor - A person who donates an organ to someone he or she does not know through a kidney exchange program so that, in turn, another living donor will give a kidney to someone that donor knows. Kidney exchange enables medically compatible donor-recipient combinations.
Other transplant words
Blood type - One of four groups (A, B, AB, or O) into which blood is classified.
Dialysis - A method of filtering the blood that tries to do the job of the kidneys. This includes removing extra fluid from the blood (which would usually leave the body as urine) and balancing chemicals (electrolytes) in the blood.
Family doctor - The doctor a person sees when he or she does not feel well or for annual medical check-ups. This kind of doctor is also called a primary care physician.
Independent living donor advocate (ILDA) -
A person who understands the organ donation process and who is not part of the transplant team. This person will:
- Promote your best interests
- Check that you have received information about:
- The informed consent process
- The tests needed to be a living donor and the risks of these tests
- The surgery, and the care you will get after the surgery
- The need to have follow-up care after donation
- Help you get more information about these topics as needed; the ILDA should not be involved with the transplant candidate
Informed consent - When a person has information about a test or procedure, understands the information, and then agrees to participate in the test or procedure.
Living donor team - The transplant hospital staff whose job is to talk with, evaluate, and protect the interests of living donors.
Medical follow-up - The requirement that living donors have medical tests a minimum of six months, 12 months, and 24 months after donation. The purpose is to make sure the donor is healthy even if the donor feels well. The transplant hospital should talk with the living donor about how and where to do medical follow-up.
Organ rejection - When a transplant recipient’s body recognizes the transplanted organ as foreign and attacks it. Acute rejection is when a person’s body mounts a sudden attack on the transplanted organ. Chronic rejection is when a person’s body slowly damages the transplanted organ over time. Both can result in organ failure.
Transplant - Surgery to take an organ from one person’s body and put into another person’s body.
Transplant candidate - A person who needs an organ transplant and who has been approved by a transplant hospital to have one.
Transplant hospital - A hospital where experienced surgeons perform organ transplants. Not all hospitals perform organ transplants.
Transplant recipient - A person who had an organ that was not working and who got an organ from a living or deceased donor.
Waitlist - Medical information about people who have been approved to get a transplant and who are waiting for an organ from a deceased donor. When an organ becomes available, a computer matches the organ with waitlist candidates based on rules designed to be fair to everyone who is waiting for an organ.



