Lung continuous distribution took effect March 9, 2023. What you need to know about OPTN lung policy changes.
Creating a new system: Goals and driving principles
The Organ Procurement and Transplantation Network is developing a more equitable system of allocating deceased donor organs. The new approach is called continuous distribution.
The goals of the new continuous distribution framework are consistent with allocation requirements in the National Organ Transplant Act (NOTA) and the OPTN Final Rule.
Continuous distribution goals
- Prioritize sickest candidates first to reduce waitlist deaths
- Improve long-term survival after transplant
- Increase transplant opportunities for patients who are medically harder to match
- Increase transplant opportunities for candidates with distinct characteristics like candidates under the age of 18 or prior living donors
- Promote the efficient management of organ placement
This new framework is being designed to allow multiple factors that contribute to a successful transplant to be considered simultaneously as part of the organ offer process.
The current system
The current system creates hard boundaries that can stop a transplant candidate from being prioritized further on the match run.
CURRENT SYSTEM: Why does it need to evolve?
Right now, a classification-based system of organ allocation is in place. The current system gives points to candidates at various steps of a sequence in the organ offer process. Candidates are transplant patients who are waiting for an organ to be offered to them.
That can mean that when certain candidate characteristics, called attributes, are reviewed in sequence, sometimes patients are placed on one side of a hard boundary that stops them from being prioritized further on the match run. The match run is the list that is generated when an organ donor’s information is entered into the national waiting list computer system, to identify potential recipients.
Some examples of a candidate’s attributes or factors include:
- Medical urgency
- Distance from the donor hospital
- Biology
- Expected outcomes
CURRENT SYSTEM: How does it work?
The current system that matches organs with patients gives points to candidates at various steps of a sequence in the organ offer process.
EXAMPLEIn this broad example, there are four candidates who are being prioritized for an organ offer: Candidates A, B, C and D.
These patients vary in terms of their:
- Medical urgency
- Distance from the donor hospital
- Candidate biology (compatibility)
- Predicted one-year post-transplant survival
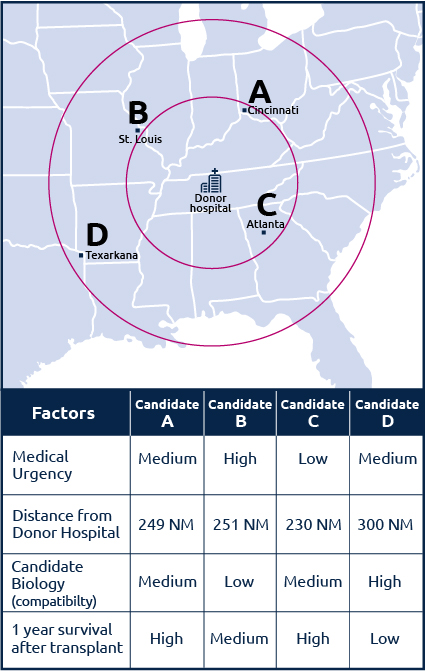
In the current classification system, any single factor could potentially determine the order in which these candidates are prioritized in a match run.
For example, if the order of prioritization were to be based first on distance, then Candidate C would receive an offer first, followed by A, B and D.
But if priority is given to the patient’s medical urgency, then Candidate B would receive the first offer, followed by A, D and C.
As this example shows, the current classification-based system sometimes places patients on one side of a hard boundary that stops them from being prioritized further, because patient factors aren’t considered together.
The new system: Continuous distribution
The new continuous distribution framework will:
- Dissolve the hard boundaries that exist in the current system
- Change how patients are prioritized by considering all patient factors together
NEW SYSTEM: How does it change organ allocation?
The new continuous distribution framework will dissolve the hard boundaries that exist in the current classification-based system. Importantly, continuous distribution is flexible enough to apply to all organ types.
Continuous distribution will change organ allocation by:
- Considering all candidate attributes at the same time, rather than placing patients into rank-ordered classifications
- Ranking candidates with an overall score that is calculated using multiple patient attributes, as well as efficiency of organ placement
Video: Organ allocation: questions and goals
Working organ type by organ type, through research and analysis, the donation and transplantation community is working together to design this framework to determine patient priority in the match run.
NEW SYSTEM: How are patients prioritized?
Continuous distribution will change how patients are prioritized. Continuous distribution will consider all patient factors togethe to determine the order of an organ offer, and no single factor will decide an organ match. The goal is to increase fairness by removing the hard boundaries that are part of the classification-based system.
Every organ type will have its own formula to calculate how candidates on the waiting list are prioritized. Depending on the formula that is chosen for a specific organ type, Candidate B in the example above may be the first to receive an offer based on a combination of high medical urgency, medium survival probability and moderate distance from the donor location.
All the factors will be considered together, but every factor will also be weighted. Depending on the weighting of the various factors, the remaining order in the example above may be A, C and D. Candidate C, with the shortest distance from the donor hospital, might appear ahead of Candidate D, who has medium medical urgency but is the farthest from the donor location.
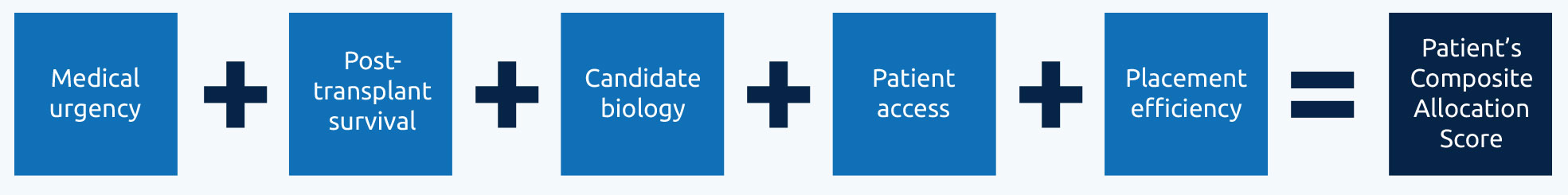
NEW SYSTEM: Points system and composite allocation scoring
Patients in the continuous distribution system will receive a composite allocation score. Attributes related to a patient’s overall score include medical urgency, expected post-transplant outcome, candidate biology, patient access and efficiency of organ placement.
A higher score puts a patient closer to the top of a match run and more likely to receive an organ transplant.

NEW SYSTEM: Attributes and the goals
Every organ type will have a specific set of attributes which will align with the goals of continuous distribution such as prioritization of the sickest candidates and increasing transplant opportunities for patients who are medically harder to match.
Visit each organ type’s continuous distribution page to learn about their specific attributes and the goals they support.
Lung Kidney and pancreas Liver and intestine HeartUnderstanding attributes and points in a match run
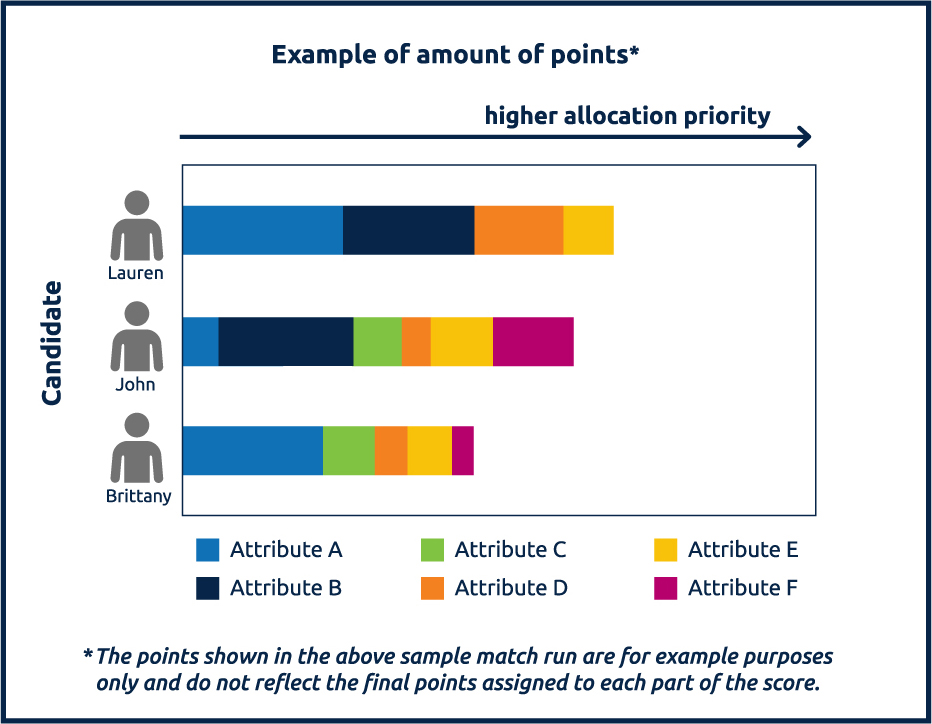
In this general match run example (not specific to any organ type):
- Each color represents a different attribute
- The length of each color indicates the amount of points given to that candidate
- The length of the bar indicates the combined composite allocation score
Candidates receive points from multiple attributes and are unique to each organ offer. In this match run example, Lauren received the most points.
In today’s allocation system, some attributes define allocation classifications. Meaning, if candidates have one of those defining attributes—for example, if they have a very rare blood type—then they will receive priority over otherwise similarly-situated candidates.
In the new continuous distribution framework, each attribute will have a specific weight, and are added together to make one composite allocation score that can change with every organ offer. A candidate’s total score will determine their prioritization on the match run.
Input will come from patients and recipients, donors and their families, and transplant professionals. Everyone has a voice.
During this process, the community will have the chance to take part in online values exercises to help decide how organ attributes are weighted and prioritized.
Developing the new system: Working together
Many decisions have to be made to develop the new system and achieve improvements for the entire donation and transplantation community. These decisions involve multiple stakeholders – patients, their loved ones, and donation and transplant professionals. Each organ-specific committee will move through the steps below to develop a policy proposal. The proposal will open for public comment before it is submitted to the Board for final approval.
How does the process work?
Community input happens at each phase of development to help shape the new system. Here are the steps we’ll take:
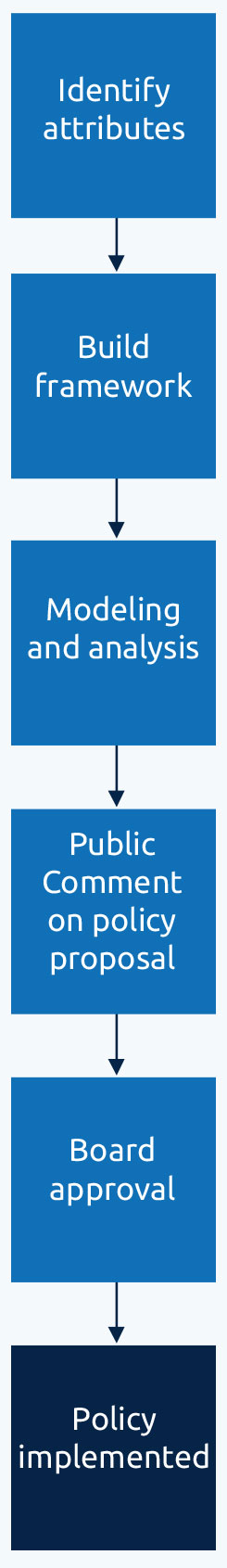
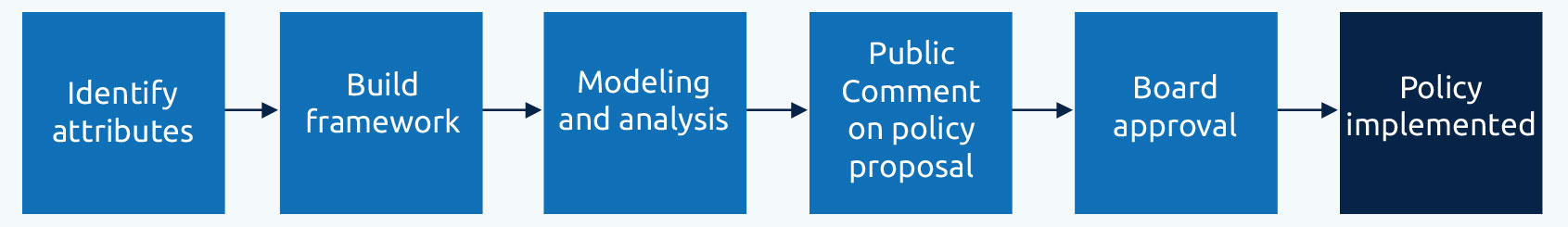
Identify attributes
This is an important first step. In each organ type’s continuous distribution framework, each attribute will be considered uniquely with regard to each candidate. Each candidate will receive points that are calculated into an overall score. Before that can happen, we must look at how candidates are currently grouped and prioritized for organ allocation. For each attribute, the committee will identify the desired policy outcomes and metrics of success.
Build the framework
The next step is to convert the organ type’s existing allocation policy into the new framework. The OPTN uses several different methodologies to develop these frameworks. Depending upon the organ, this can include a combination of the following steps:
- Align attributes: Every attribute aligns with one of the five goals, mentioned above, that are in alignment with NOTA and the Final Rule. We then use clinical data to compare attributes with similar goals.
- Convert attributes into points: For each attribute considered toward the overall score, a decision will be made about how to assign points to candidates according to differences in the attribute. For example, how many points do we give to blood type A versus O? 100 miles versus 1,000 miles?
- Conduct sensitivity analysis: A sensitivity analysis is an analysis used to measure the impact of a change to a single variable. For example, if a change is made to the weight of any attribute, the new match run will be shown as the outcome. Sensitivity tools will be built for each organ type to evaluate continuous distribution. The tools will be made publicly available as part of the development process.
Explore the lung sensitivity tool - Prioritize attributes against each other: The specific weight of each attribute determines how much influence it will have toward the overall score. This step can include any of the following analyses:
- Community input collected through online values exercises. Values exercises show each participant a pair of attributes that will be used to prioritize candidates. The participant must decide if all else is considered equal, which attribute is more important than the other when prioritizing a candidate for an organ. Learn more about how values exercises work
- A revealed preference analysis to review how multiple decisions have been made in the existing organ allocation system. For example, how important was distance compared to waiting time when a decision was made between two candidates? The analysis will take the current system and create a baseline to be measured against.
Read: Revealed preference analysis for lung (PDF) - Mathematical optimization to help identify policy scenarios that meet the policy outcomes expressed by the community and required by federal law. Read: paper on mathematical optimization for continuous distribution
Modeling and analysis
Scientific Research and Transplant Registry (SRTR) modeling and results: The SRTR works with the OPTN to provide analytic support for policy development. Their researchers will take the proposed policies and model them to understand how they could impact candidates. This will help identify any potential unintended consequences or harmful outcomes. The SRTR modeling results will also estimate the benefit of the new proposal and inform any needed improvements.
Public comment on policy proposal
This step involves considering the community input received, modeling and analysis, as well as the committee project work, to develop and propose a new composite score as a policy proposal for public comment. See details around the policy development process, including public comment.
Board approval
After the Board of Directors approves the proposal with the new framework, plans for implementation begin.
Implementation
As each organ moves into continuous distribution, implementation of the approved policies is projected to take approximately 12 months due to the range of changes, required education to the community, and expected impact.
NEW SYSTEM DEVELOPMENT: Progress by organ
The continuous distribution framework will be flexible enough to apply to all organ types. Using the same framework for all organs will improve organ allocation by creating consistency and transparency for the entire transplant community.
The current organ matching process is different for each organ type. To develop a framework that works for each organ, we will look at each organ type individually.
| Organ | Expected start |
|---|---|
| Lung Implemented March 9, 2023 | January 2019 |
| Kidney and pancreas | June 2020 |
| Liver & intestine | December 2021 |
| Heart | January 2023 |
| Vascularized Composite Allograft | To be determined |
Take action and help build the framework
Continuous distribution is the future of organ allocation. Your input is critical to the process of developing a consistent framework that is best for patients.
The entire community can participate in several ways:
- Add your voice to public comment, which happens twice a year and is an essential part of the policy development process
- Attend a regional meeting
- Participate in a values exercise to help prioritize attributes
Values prioritization exercises
These exercises are helping inform the development of the framework for each organ type. Participants are asked to compare two attributes against each other and select their level of importance when considering a candidate for organ transplant. This information will be used to inform the weight of each attribute and the overall score.
We encourage all members of the donation and transplantation community, including donors, patients and their loved ones, to participate in these important values exercises.
Each organ type will have a values exercise. The results of the exercises will be used to inform each organ committee as they develop frameworks for each organ type. The methodology, Analytic Hierarchy Process (AHP), has been used effectively by other healthcare groups to involve patients in making clinical decisions.
Watch this instructional video to learn more about the OPTN community values prioritization exercise.
| Organ | AHP exercise |
|---|---|
| Lung | Was open during summer 2020 public comment and closed on Oct. 1, 2020. |
| Kidney | Was open during winter 2022 public comment and closed on March 23, 2022. |
| Pancreas | Was open during winter 2022 public comment and closed on March 23, 2022. |
| Heart | Was open during winter 2024 public comment and closed on March 19, 2024. |
Background & resources
In December 2018, the OPTN approved a continuous distribution model as a framework for developing future organ allocation policy, upon the recommendation of a specially called Ad Hoc Geography Committee. Continuous distribution was selected after consideration of multiple alternative frameworks and was developed with input from the public and the transplant community. Recent changes to organ allocation have been made in an effort to align with this new framework and improved equity in organ allocation. Visit the Ad Hoc Geography Committee page for more information about their recommendations.
Glossary
Allocation
The process of determining how organs are distributed. Allocation includes the system of policies and guidelines that ensure that organs are distributed in an equitable, ethical and medically-sound manner.
Allocation policies
Rules established by the OPTN to guide and regulate organ allocation and distribution in the U.S.
Analytic Hierarchy Process (AHP)
A multi-criteria decision-making methodology. The OPTN is using AHP to help gather information for the development of continuous distribution. Participants in AHP exercises are asked to make decisions about the relative importance of organ attributes when compared to each other.
Attribute
An attribute is a quality or characteristic of something. In organ allocation, attributes are criteria used to classify and sort and prioritize candidates. For example, in lung allocation, attributes include medical urgency, travel mode, ischemic time, blood type compatibility, and others. Each organ type will have its own attributes in continuous distribution.
Candidate
A person registered on the organ transplant waiting list.
Classification-based framework
A classification-based framework groups similar candidates into classifications or groupings. Candidates are then sorted within those classifications. A candidate will only appear in the classification that is most beneficial to them. This is the framework currently used to allocate organs.
Cold Ischemic Time
The amount of time an organ spends being preserved after recovery from the donor.
Composite Allocation Score
A composite allocation score combines points from multiple attributes together. Continuous distribution uses composite allocation scores in a points-based framework.
Distribution
The way something is shared across a group or area.
Framework
The collection of policies and procedures used to distribute organs. Examples include concentric circles and continuous distribution.
Match run
A computerized ranking of transplant candidates based on donor and candidate medical compatibility and criteria defined in OPTN policies.
Points-based framework
A points-based framework gives each candidate a score or points. Organs are then offered in descending order based on the candidate’s score. Continuous distribution of organs involves a points-based framework.
Weight
Weights are the relative importance or priority of each attribute toward our overall goal of organ allocation.



